A research team led by the Department of Paediatrics and Adolescent Medicine, School of Clinical Medicine, LKS Faculty of Medicine, the University of Hong Kong (HKUMed), has conducted a pioneering study that established a causal link between childhood maltreatment (CM) and various neuropsychiatric disorders. By employing genomic analysis on neuropsychiatric data from over 500,000 individuals and CM data from over 140,000 cases, the study found that CM victims face a nearly five-fold increased lifetime risk of developing schizophrenia. Furthermore, the findings indicate that CM significantly elevates the risk of multiple neuropsychiatric disorders through altered behavioral patterns, cognitive abilities, and genomic changes, providing the scientific evidence for developing more precise early intervention and prevention strategies. The study was published in The British Journal of Psychiatry. (link to the publication)
Childhood maltreatment: A global concern with a 60% rise in Hong Kong
The World Health Organisation designated CM as a global public health challenge, encompassing various forms such as physical abuse, emotional abuse, sexual assault and neglect. The situation in Hong Kong is also cause for concern. According to the Social Welfare Department, newly reported CM cases surged from 940 in 2020 to 1,504 in 2024, representing a 60% increase. Research indicates that maltreated children are more prone to social interaction difficulties, attention deficits, and disruptive or aggressive behaviours during development. However, these early warning signs are often overlooked. Failure to identify or intervene promptly can allow problems to escalate, potentially deteriorating into severe mental disorders and imposing a substantial healthcare and economic burden on society. Against this backdrop, Hong Kong's upcoming implementation of the Mandatory Reporting of Child Abuse Ordinance in January 2026 underscores the urgent need for enhanced child protection measures.
By integrating large-scale genomic datasets from the UK Biobank and the Psychiatric Genomics Consortium, the research team analysed neuropsychiatric data from up to 500,000 individuals and CM data from over 140,000 people. This effort successfully established a causal link between CM and multiple neuropsychiatric disorders, while identifying key risk factors and genetic marks associated with increased susceptibility to such disorders.
Childhood maltreatment leaves genetic marks that heighten mental health risks for life
The findings revealed that individuals experiencing CM face markedly elevated mental health risks: a five-fold increased risk of schizophrenia, up to nine times higher risk of attention deficit hyperactivity disorder (ADHD), and nearly double the risk of major depressive disorder. At the biological level, the study discovered that CM leaves epigenetic markers on the genome known as ‘DNA methylation'. These markers, which can be influenced by environmental factors, lifestyle habits, and even psychological stress, represent long-term epigenetic scars triggered by CM. Among thousands of such markers, researchers pinpointed ten genetic locations near nine critical genes. Notably, three of these genes—CLU, MAPT and HNRNPK—are associated with neurodegenerative diseases, including Alzheimer's disease, Parkinson's disease, and other cognitive disorders. This finding suggests that CM may affect some of the same biological pathways that are involved in both neuropsychiatric disorders and neurodegenerative diseases.
Dr Brian Chung Hon-yin, Clinical Associate Professor, Department of Paediatrics and Adolescent Medicine, School of Clinical Medicine, HKUMed, explained, ‘Conventional studies rely primarily on long-term follow-ups and questionnaires, which are susceptible to confounding factors, such as one's environment and social background. These confounders make it challenging to accurately evaluate the long-term impacts of CM, leading to a lack of strong evidence for policy-making and clinical intervention. Our team is the first to employ genomic and epigenomic methods, using a hypothesis-free approach to analyse how CM influences the brain and gene expression, thereby identifying opportunities for intervention and providing a foundation for prevention and treatment.'
Dr Chung added, ‘Our research demonstrates that CM can leave long-term genetic marks and affect genes related to neurodegenerative diseases. By identifying specific DNA methylation markers, we aim to develop early biomarker screening for high-risk populations in the future and even explore novel therapeutic targets for drug development to reduce disease risk at the source. This study serves as an important first step. Moving forward, we will apply the same rigorous methodology to systematically examine a broader spectrum of early-life adversities such as abuse, neglect, and family dysfunction to comprehensively analyse their overall harm and long-term impact, ultimately seeking to drive societal awareness and action on the profound effects of early-life adversities on mental health.'
Professor Cheung Yiu-fai, Chairperson of the same department, commented, 'This study clearly demonstrates that genomic medicine is no longer confined to rare diseases. By applying the rigorous Mendelian randomisation method, which is ranked just below randomised controlled trials in the evidence hierarchy, our genomics team has discovered causal pathways linking CM to common neuropsychiatric conditions. This research represents a paradigm shift in the field, and highlights the potential of genomics to deliver robust, actionable insights to address complex challenges in paediatrics and public health.'
Three modifiable factors identified to mitigate risks
The study further revealed that the impact of CM extends beyond direct psychological harm. It increases neuropsychiatric risk through three mediating factors: addiction-related behaviours (such as smoking initiation, prolonged screen time, and substance abuse), cognitive traits (like executive functioning, intelligence, and risk tolerance), and socioeconomic factors, such as educational attainment.
Dr Chung explained, 'While the influence of these factors varies across different neuropsychiatric disorders, they are all modifiable. Interventions aimed at improving behaviours, enhancing cognitive ability, and providing educational support during development can effectively lower the risk. However, the long-term epigenetic markers left by CM are near genes associated with neurodegenerative diseases, and may be difficult to reverse. Therefore, preventing CM remains the most fundamental strategy for protecting children.'
About the research team
The research was led by Dr Brian Chung Hon-yin, Clinical Associate Professor, Department of Paediatrics and Adolescent Medicine, School of Clinical Medicine, HKUMed. Other team members include Dr Christopher Mak Chun-yu, MPhil graduate Nicole Ng Ying-ting, and PhD candidate John Tang Yen, all from the same department; and Professor Jane Zhao Jie, Assistant Professor, School of Public Health, HKUMed.
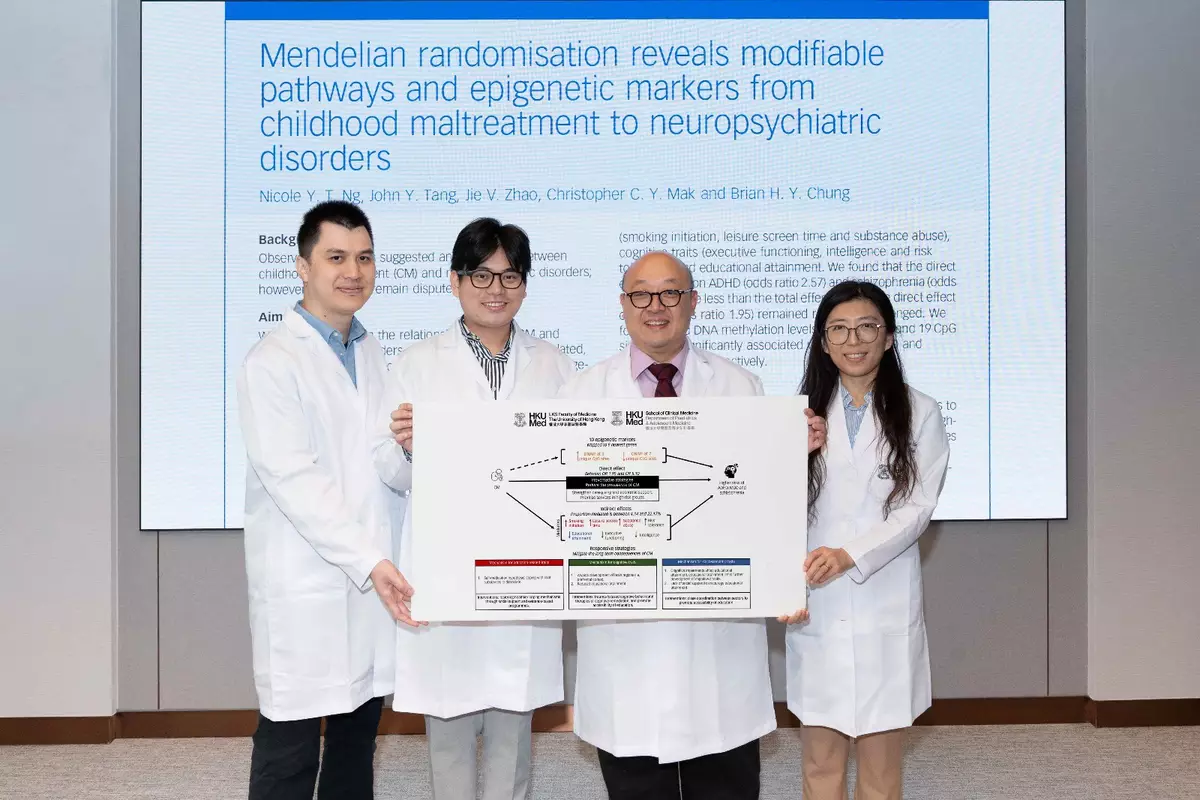
A research team led by Dr Brian Chung Hon-yin (third left) has revealed that individuals who experienced childhood maltreatment face markedly elevated mental health risks.
Dr Brian Chung Hon-yin (front left) stated that the long-term epigenetic markers resulting from childhood maltreatment (CM) are near genes associated with neurodegenerative diseases, and may be difficult to reverse. Therefore, preventing CM remains the most fundamental strategy for protecting children.