Liver cancer is the sixth most common cancer worldwide and the third leading cause of cancer-related deaths. A recent report published in 'The Lancet' predicts that the number of new liver cancer cases will increase from 870,000 in 2022 to 1.52 million by 2050, nearly doubling the figure. If the current trend continues, this increase could result in 1.37 million deaths.
Traditional cancer therapies often overlook patient-specific and dynamic tumor immune environments, causing ineffective treatments, toxic side effects, and critical delays. The University of Hong Kong (HKU) has developed 'Liver-in-Cube', the world's first 3D-bioprinted platform that precisely reconstructs the liver cancer microenvironment in the lab using a patient's own cells and extracellular matrix. This platform offers a fast and reliable service to help patients identify the most effective personalised treatments and pave the way for a standardised, high-throughput solution for drug assessment and development.
The invention can accurately simulate tumour characteristics of individual patients, such as the cell numbers, tissue stiffness and immune microenvironments, enabling doctors to swiftly assess the efficacy and side effects of various drugs and emerging therapies, leading to more precise treatment decision. This technology has received the ‘Gold Medal’ at the International Exhibition of Inventions of Geneva, ‘Special Grand Prize’ at Prize of the China Invention Association, and ‘Best-Performing Start-Up Award’at Asia Summit on Global Health (ASGC) Conference.

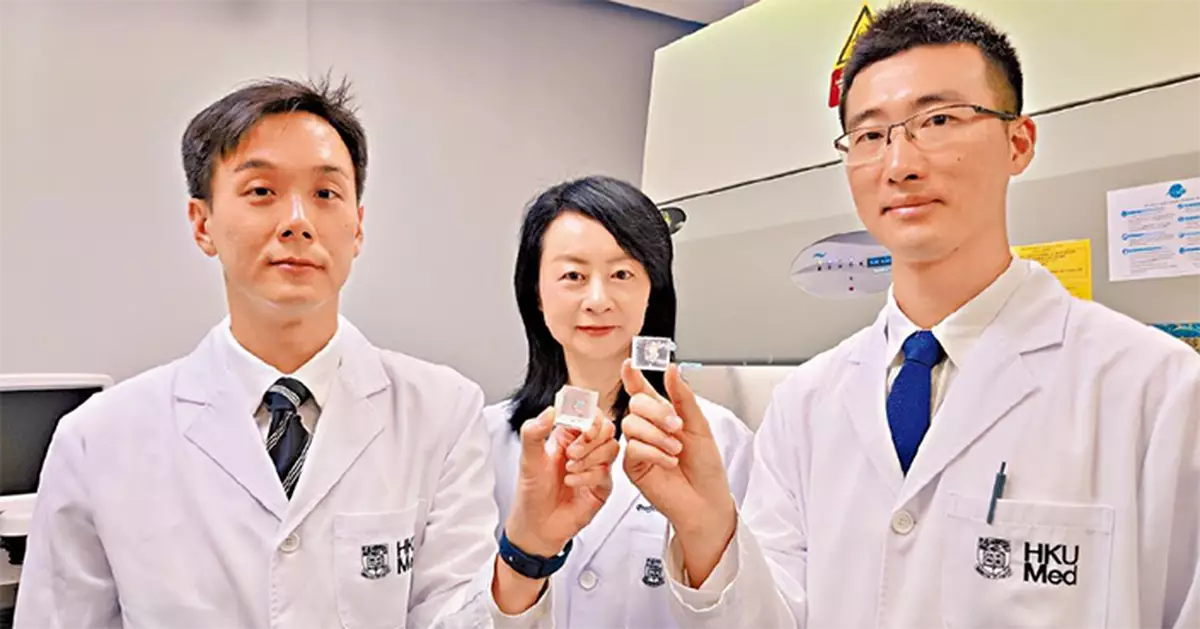
The technology has received the ‘Gold Medal’ at the International Exhibition of Inventions of Geneva, ‘Special Grand Prize’ at Prize of the China Invention Association, and ‘Best-Performing Start-Up Award’at Asia Summit on Global Health (ASGC)Conference. Photo source: HKUMed
From ‘Trials to Tailored Treatment’: Seizing the Golden Treatment Window
Currently, there is a lack of personalised drug-screening platforms for liver cancer treatment in the market, which often makes patients undergo multiple treatment failures in the search for the most suitable drug. This not only imposes a heavy financial burden but may also delay the timing in killing the tumour cells effectively. The 'Liver-in-Cube' directly addresses this pain point by accelerating the evaluation of the efficacy and side effects of various drugs for patients, allowing doctors to identify the optimal treatment method for patients and reducing the risk of cancer recurrence due to treatment delays. The ‘Liver-in-Cube' has now started patient recruitment at local hospitals to expedite clinical trials and advance its transition into clinical application.
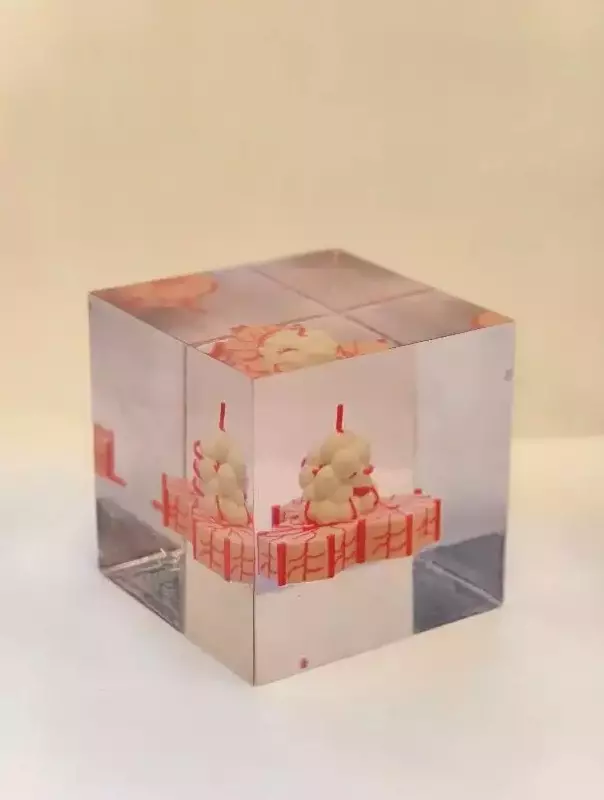
The 'Liver-in-Cube' developed by HKU, Photo source: HKUMed
Dual Value in Clinical and Research Excellence
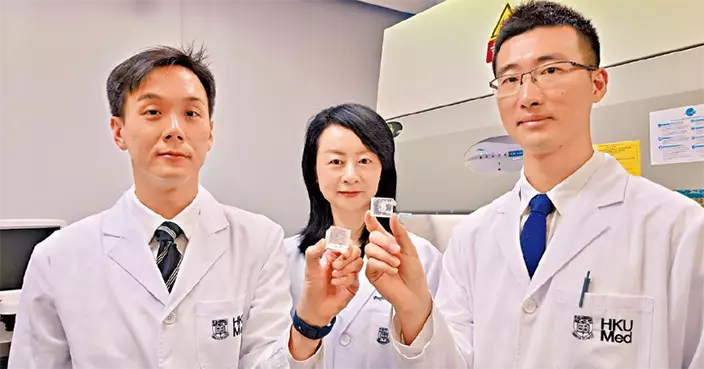
Professor Man Kwan, Chair Professor in the Department of Surgery, School of Clinical Medicine, HKUMed, who led the research project, stated that ‘Liver-in-Cube' can speed up the identification of the most effective drugs for patients, significantly enhancing treatment efficiency and reducing side effects, with the potential to greatly improve patient survival rates. In pharmaceutical development, the technology serves as a substitute for animal models, accelerating preclinical efficacy and safety testing for new drugs with more accurate data to increase the success rate of further clinical trials. This invention can shorten the new drug development cycle with reducing costs. In the field of basic research, the model assists researchers in exploring immune regulation mechanisms and discovering new therapeutic targets and strategies. The application prospects of the ‘Liver-in-Cube' are extensive, and its technological framework can be expanded to other liver diseases and cancers, promoting the widespread adoption of precision medicine. Currently, the technology is undergoing clinical trials in local public and private hospitals. The team aims to leverage the scientific data to facilitate the commercialisation of the technology and make it available in both local and overseas markets, thus benefitting a wide range of patients.
The University of Hong Kong (HKU) has developed‘Liver-in-Cube’,the world’s frst 3D-bioprinted platform that precisely reconstructs the liver cancer microenvironment in the lab using a patient’s own cells and extracellular matrix. Photo source: HKUMed
Five core technologies of ‘Liver-in-Cube':
• 1. Novel Technology for Cell and Matrix Protein Separation: Simultaneously extracts hepatocytes, tumor cells, immune cells, and matrix proteins from the tissue of the liver cancer patient, accurately simulating individual tumor characteristics.
• 2. Advanced 3D Bioprinting: Creates a biomimetic model incorporating normal tissue, tumor tissue, and vascular structures, surpassing traditional 3D cell culture and organoid products in reproducing a patient's tumor architecture.
• 3. AI-assisted patient parameterisation and printing: Utilising AI models trained on clinical biobanks, we correlate pathological features, tissue stiffness, and tumor immune microenvironment subtypes to determine the optimal geometric structure and bio-ink composition for each patient.
• 4. Customised patient-specific tumor characterisation system: By precisely measuring patient-specific parameters such as tumor stiffness and immune profiles, we reconstruct a highly biomimetic, individualized tumor microenvironment for each patient.
• 5. Innovative Tumor Model with Microvascular System: Enables continuous drug testing and evaluation of various therapies, enhancing the assessment of treatment effects in a laboratory setting.
Led by Professor Man Kwan from the Department of Surgery, HKUMed, the research
team focuses in the study of postoperative recurrence and immune microenvironment
of liver cancer. Over the decades, the team has become internationally recognised as
the leading force in the fields of liver oncology, transplant oncology, and transplant
immunology.